Ever stared at your long-term care insurance policy wondering why something so crucial was left out when you needed it most? Yeah, us too. Let’s face it—Coverage Exclusions feel like that one ingredient missing in your favorite recipe. Except this one costs way more than salt.
In this post, we’ll dig into the nitty-gritty of long-term care insurance, demystify those pesky exclusions, and arm you with actionable steps to avoid unexpected surprises. You’ll learn what coverage exclusions mean for your policy, how to decode them, tips to protect yourself, real-life examples of how these exclusions play out, and much more. Think of this as your ultimate guidebook to financial preparedness!
Table of Contents
- What Are Coverage Exclusions, Anyway?
- Decoding Your Policy Like an Expert
- Smart Tips to Navigate Coverage Exclusions
- Real-World Stories That Hit Hard
- FAQs About Long-Term Care Insurance Exclusions
Key Takeaways
- Coverage exclusions are specific conditions or scenarios where insurers won’t pay despite having a policy.
- Common exclusions include pre-existing conditions, self-inflicted injuries, and treatments deemed non-medically necessary.
- Reading the fine print is vital; skipping it can lead to costly mistakes.
- Work with licensed agents to clarify terms before making decisions.
What Are Coverage Exclusions, Anyway?

Alright, let’s break down the big bad wolf here: coverage exclusions. Imagine spending years dutifully paying premiums only to find out that your policy doesn’t cover Alzheimer’s care because of some weird clause no one bothered explaining. That’s an exclusion—a situation where the insurer isn’t obligated to pay benefits.
Why do they exist? Simple: Insurers need rules to keep risks (and payouts) manageable. But here’s the kicker—these exclusions aren’t always clear unless you’re actively looking for them.
Optimist You:
“It’s just legal jargon—it’ll never happen to me!”
Grumpy You:
“Ugh, sure, until it does.”
Decoding Your Policy Like an Expert
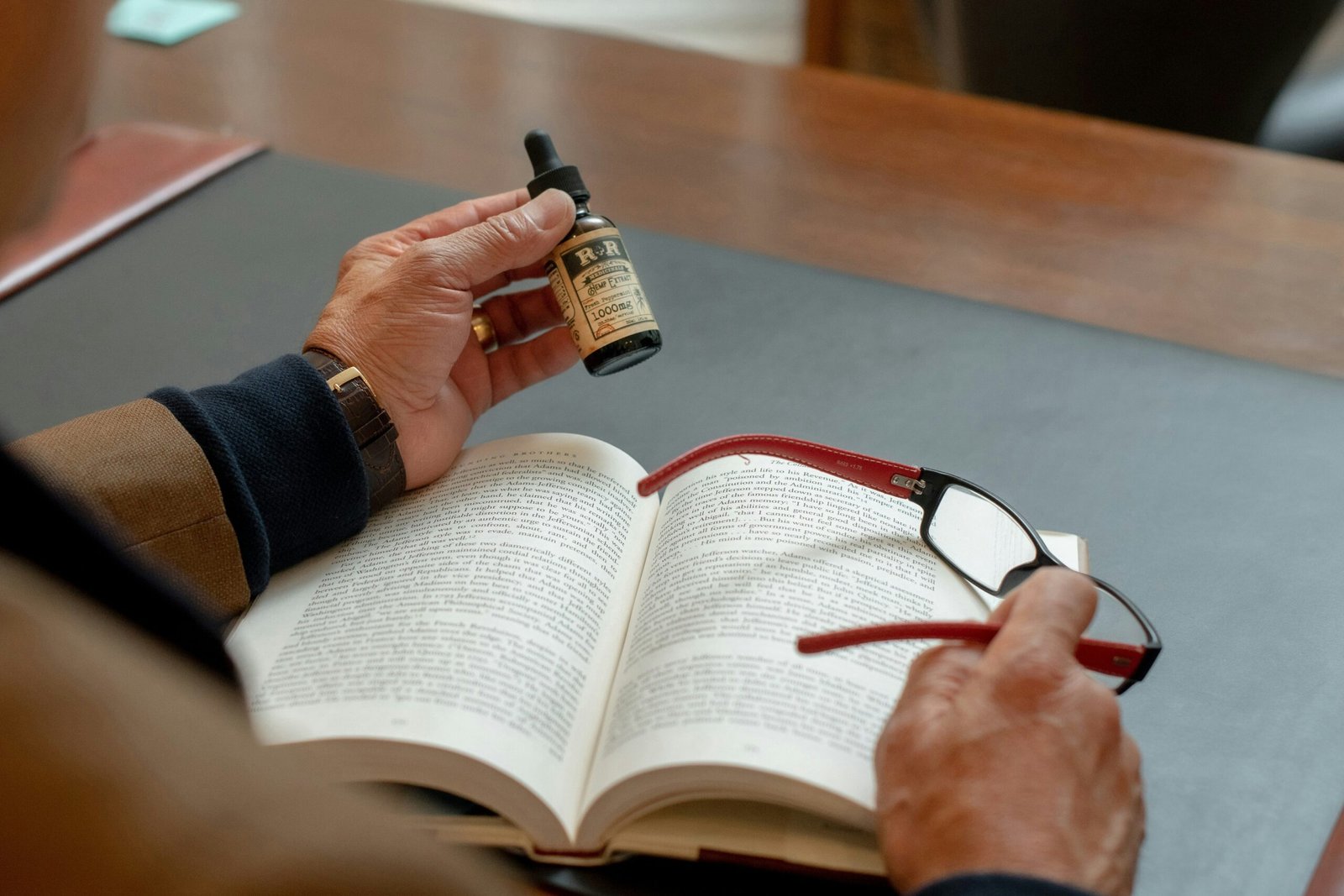
I once skimmed over a “pre-existing conditions” section thinking, *How could I possibly miss this detail?!* Spoiler alert: I did. And guess what? When my elderly uncle had a stroke two months after his policy started, his claim got denied faster than you can say “exclusion clause.”
This mistake cost us dearly—not just in money but in stress. If I’d taken time to decode the fine print, maybe things would’ve turned out differently. To help YOU avoid my epic fail, here’s what to look for:
- Pre-Existing Conditions: Many policies exclude claims related to health issues already diagnosed within a certain timeframe.
- Mental Health Disorders: Some insurers refuse coverage for mental illnesses altogether. Yep, you read that right.
- Non-Medical Treatment Services: Ever dreamed of hiring a masseuse as part of rehab? Nope, not covered.
Sounds harsh, right? Like biting into an apple pie without cinnamon—it looks okay, but something feels off.
Smart Tips to Navigate Coverage Exclusions
1. Ask Questions—LOTS Of Them!
Seriously, treat your agent like Google Assistant. If they dodge a question, ask again louder (or switch agents). A good agent will walk you through every line item so there are no nasty surprises later.
2. Compare Policies Sideways—and Upside Down
Different insurers handle exclusions differently. While one might nix home-care benefits entirely, another could offer limited inclusion. Use comparison tools to identify the best fit for YOUR needs.
Terrible Tip Alert:
“Just go with the cheapest option.” Newsflash: Low premiums often = hidden costs. Don’t fall for it.
3. Document EVERYTHING
From conversations about your policy to receipts for medical expenses, save everything. One day, those notes may become your saving grace during disputes.
Real-World Stories That Hit Hard
Rachael from Texas thought her long-term care plan was foolproof…until her husband developed dementia. Unfortunately, their policy included a blanket dementia exclusion buried deep in paragraph 47. With mounting bills and rejected claims, Rachael found herself working twice as hard past retirement age just to stay afloat.
On the flip side, Mike from Ohio worked tirelessly upfront to understand his mother’s policy—and caught a sneaky loophole involving custodial care limits. By addressing discrepancies early, he saved his family thousands down the road.
Which story sounds better to you?
FAQs About Long-Term Care Insurance Exclusions
Q: Can I negotiate exclusions on my policy?
A: Rarely. However, switching providers or bundling services might open doors to wiggle room.
Q: Do all insurers have the same exclusions?
A: Nope! This is why research pays off.
Q: Will Medicare cover what my insurance doesn’t?
A: Sadly, not usually. Medicare focuses on short-term care, leaving gaps many don’t realize till it’s too late.
Conclusion
Long-term care insurance is more than signing paperwork—it’s understanding exactly what you’re buying. By tackling coverage exclusions head-on, asking tough questions, and documenting every step along the way, you position yourself ahead of potential disasters. After all, nobody wants to relive my uncle’s denial nightmare—or be stuck navigating life without proper preparation.
And now, as promised, here’s a little cherry on top:
Coverage plans, Exclusions bite. Read fine print tight— Your future brightens overnight.